What Happens Next and When
What Happens Next and WhenWhat Happens Next and When
As treatment comes to an end, you and your family can start to transition out of treatment mode and into more familiar routines while the healthcare team continues to monitor your child’s recovery. The end of your child’s neuroblastoma treatment is a joyous milestone and something to be celebrated. After months of therapy, you, your child, your family, and loved ones should recognize and celebrate this achievement.
Jump to a section below to learn more:
The Importance of After Treatment Follow-up
Hear from a pediatric oncologist and nurse practitioner about why long-term follow-up is important for your child after they complete their treatment journey.
Learn about the transition from treatment
Find answers below to common questions that caregivers have at each stage of the transition.
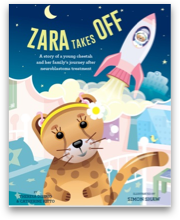
Becoming their own advocate
As the years go by and your child grows older, it will be important for them to be aware of their unique medical needs. Teaching them over time about neuroblastoma and their specific journey will increase their awareness and readiness to take ownership of their health. Having an updated treatment summary and care plan that they can share is key in helping them make sure they get the care they need.